Devastating Effect on Minority Communities
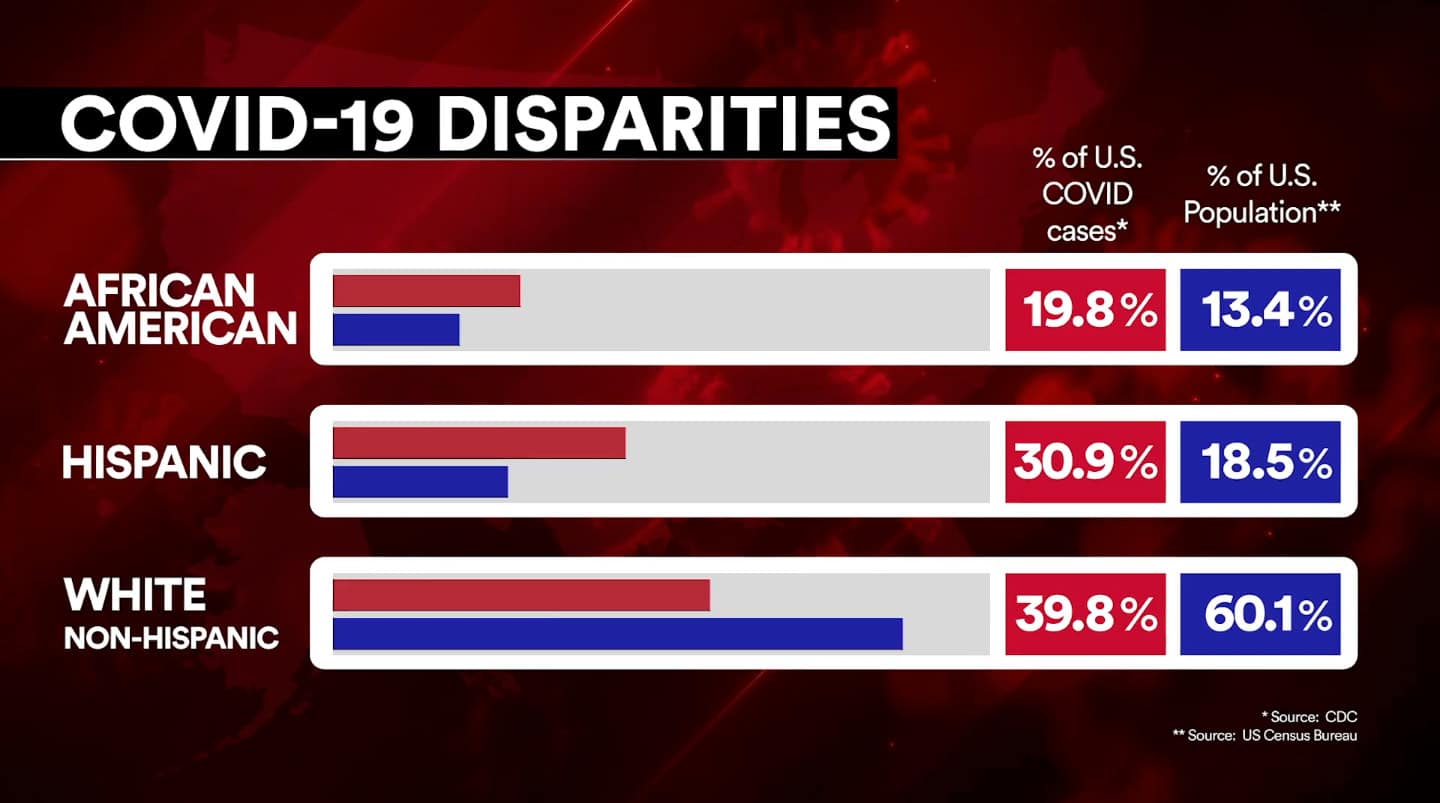
It is no secret that COVID-19 has had a devastating effect on minority communities throughout the United States. For anyone doubting that claim, there are statistics like these to prove further these claims correct. From this study, groups like African-Americans, indigenous Americans, African-Americans, Latinos, and Pacific Islanders have experienced a COVID-19 death rate of double or more than whites. That is not to say whites haven’t been devastated by the impact of COVID-19 throughout America. Still, by analyzing actual data rather than just simply reading headlines, it is clear to see these groups are being hammered by the virus and could help shine a light on racial health equity throughout Detroit and the rest of the country.
COVID-19 Deaths By Race and Ethnicity in the United States
Pacific Islander, Latino, Indigenous, and Black Americans all have a COVID-19 death rate of double or more than White and Asian Americans, who experience the lowest age-adjusted rates.
From the Start of the COVID-19 Pandemic:
- 1 in 680 Latino Americans has died (or 147.3 deaths per 100,000)1
- 1 in 555 Black Americans has died (or 179.8 deaths per 100,000)1
- Indigenous Americans have the highest actual COVID-19 mortality rates nationwide1
Key Statistics Regarding the Effect of COVID-19 on Minority Groups:
- Nationwide, Black people are 2.0 times more likely to have died than White people and 2.1 times more likely to have died as Asian people when age is taken into account.1
- Nationwide, Indigenous people are 2.2 times more likely to have died than White and Asian people when age is taken into account.1
Examining and Addressing COVID-19 Racial Health Equity Disparities in Detroit
based on a local study (Detroit), in an area heavily populated by African-Americans, we should focus on our content topic. Going back to the previous link, an eye-catching quote introduced in the article – “Blacks are 2.1 times more likely than whites to die from the virus. In fact, if Blacks had the same death rate as whites from COVID-19, roughly 25,000 fewer Black people would have died in 2020.”, shines a light on the impact the virus has had on the black community. In a heavily populated area like Detroit, with a large population of African-Americans, blacks represent over 75% of COVID diagnoses by all races and makeup nearly 90% of the death toll. As the article notes, there is still missing data, so the black community could be hit even harder than we already know of. What factors are causing blacks to suffer more from the virus than whites? The black community in metro-Detroit is more likely to struggle with housing, income, and lack of food access than whites in this community. Another interesting note –“ A majority of parents report significant struggles with education for their children during the pandemic and report low levels of confidence in the school system to handle these challenges.” This could be a relatively silent factor that most may not recognize as a key contributor to the hardships the black community faces from the virus.
.@LWileden, @FordSchool @UMSociology PhD candidate, joins others in a report published by @BrookingsInst, "Examining and addressing #COVID19 racial disparities in Detroit": https://t.co/f23NCEBglM. pic.twitter.com/YPPVQDlMH3
— Ford School (@fordschool) March 8, 2021
Health Disparities the Black Community is Facing
- Black residents are significantly more likely than Whites to report not having enough money to pay their bills and take out loans relative to Whites. In fact, Blacks are 40% more likely to report that they run out of money. Over 75% of Detroiters make under $50,000 a year.2
- Black residents in Detroit relative to White residents are significantly more likely to report challenges in securing and maintaining housing, obtaining medication, and getting food, water, and other household supplies.2
- Black residents report spending more money on food and gas during the pandemic and obtaining food from local food banks. With children engaging mostly in remote learning, parents are concerned with providing more food with less money. Black Detroiters report being more likely to have children living in the home.2
Studies from heavily-populated regions throughout the United States, especially those with a high population of African-Americans, can help provide more intel on the factors leading to the higher-likeliness of Covid-related deaths from African-Americans in comparison to whites, especially in Detroit.
Health Equity Considerations and Racial and Ethnic Minority Groups
The CDC is perhaps the best source to collect intel/data from on this topic. There is a clearer picture of why minority groups are at an increased risk of contracting, getting sick from, and dying from COVID-19. Factors include “discrimination,” which stems from health care issues, housing, education, criminal justice, and finance.
The topic of racism in general throughout the United States “can lead to chronic and toxic stress and shapes social and economic factors that put some people from racial and ethnic minority groups at increased risk for COVID-19”3. The other factors can be associated with increased cases, hospitalizations, and deaths in minority-dense areas. “Besides, community strategies to slow the spread of COVID-19 may cause unintentional harm, such as lost wages, reduced access to services, and increased stress, for some racial and ethnic minority groups”. Simply put, lack of access to certain resources will further put you at risk regarding the virus’s effects.
It’s not breaking news that minority groups across America have large percentages of their individual populations deprived of these resources. This seems to be a product of systematic injustices that have been prevalent throughout the history of our country. It’s important to add in that the CDC has a “What We Can Do” section that provides “solutions” to combat this issue and, to the very least, minimalize the spread of the virus in general, which in turn can benefit these impoverished groups. While this section doesn’t necessarily reflect on our current content, the “solutions,” for the most part, are self-explanatory – support one another, continue to practice social distancing guidelines, work with community organizations, employers/healthcare systems/public health agencies/etc.

COVID-19 and the Minority Disparities in Health Care
Building upon the evidence that minority groups are more likely to get sick and die from the virus, this article is more related to healthcare. They list reasons why minorities are facing healthcare-related barriers. The reasons include lack of health insurance (expensive healthcare prevents them from getting treatment), limited access to testing (requires you to have a doctor in the first place, and some may not even own a vehicle that would allow for drive-thru testing), lower quality of care & “unconscious discrimination” (the article attributes these to systematic racism), poor communication due to language/cultural barriers, and “lack of trust” from minorities stemming from past racial equity issues.
- “Racism is a system that ensures racial inequality,” says Gilbert Gee, Ph.D. professor of community health sciences at the University of California, Los Angeles. It happens at different levels. In institutional racism, the discrimination occurs within an organization, such as the health care system.”4
- One survey found that half of the white medical students believe myths about Black people, such as they have thicker skin or less sensitive nerve endings than white people.4
- Doctors tend not to prescribe pain medicines to minorities as often. In one study of emergency rooms, Black patients were 40% less likely, and Hispanic patients were 25% less likely to get acute pain drugs.4
References
- “The Color of Coronavirus: COVID-19 Deaths by Race and Ethnicity in the U.S.”, APM Research Labs Staff, https://www.apmresearchlab.org/covid/deaths-by-race
- “Examining and addressing COVID-19 racial disparities in Detroit”, Rashawn Ray, Jane Fran Morgan, Lydia Wileden, Samantha Elizondo, and Destiny Wiley-Yancy, https://www.brookings.edu/research/examining-and-addressing-covid-19-racial-disparities-in-detroit/
- “Health Equity Considerations and Racial and Ethnic Minority Groups”, CDC, https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html
- “COVID-19 and the Minority Disparities in Health Care”, WebMD, https://www.webmd.com/diabetes/minority-health-20/minority-health-care-disparity
MediSite, Inc. is a health analytics platform based in Michigan.
StoreFRONT is our real-time transaction monitoring system supporting early detection and intervention for high-risk urban minority populations during COVID-19.

